Great article Anoop.
What should fitness professionals understand about pain and injury?
January 08 2014
I wrote an article a couple of years back to introduce fitness professionals to the new revolution in the understanding and treatment of pain. Despite making some progress forward, I think there still remains some confusion and misunderstanding about the relationship between pain and injury. It goes without saying that pain is a topic that fitness professionals should have a better understanding. I have tried to include a few questions that I feel trainers and strength coaches might have trouble with. So without further ado, here we go:

What is this whole talk about how injury and pain are not related and how pain is in the brain? Is it true? If so, I don’t get it.
We used to believe (some people still do) pain and injury to be highly correlated and would utilize the measure of pain as an indicator of tissue damage. Unfortunately, as we begin to learn more about pain and injury, it is clear that pain is not an accurate indicator of injury nor damage. To understand this better, we have to understand a very important concept. So pay attention.
Pain does not (technically) begin at the level of the tissues: While we once thought pain to originate at the level of the tissue (and that “pain” information was carried up to the brain), we now understand that these carriers, nociceptors, relay “danger” information to the brain for processing. . Once the “danger” information reaches the brain, it is then up to the brain to decide whether these signals are dangerous enough to respond by producing an output of pain. So we don’t have pain receptors or ascending pain pathways as we commonly thought. Pain doesn’t begin until the brain determines it is needed.
It is crucial that we understand this response is quite individual. One may have a very serious injury and complain of little to no pain, while another may have a very minor injury and experience extreme pain. The degree of injury is not always related to the degree of pain. Hence they say, injury and pain are not related and ‘pain is in the brain’.
But what makes the brain think it is indeed threatening or I am in danger, and let’s generate some pain?
Well, many things, actually. Your attitudes, beliefs, past experiences, knowledge, social context, sensory cues, nociception and so forth may all be confounding variables influencing your brains decision. What we have to understand is nociception is just only one of many inputs that the brain assesses to see if it is indeed in danger. Pain is only generated if the brain concludes that body is in danger and action is required.
This is bull crap; are you telling me if I cut my hand, I won’t feel pain? .
A lot of people who are resistant to accepting this concept may only be considering examples where they had injury and then felt pain. A=B. Unfortunately, this relationship isn’t as clear as we may think. We may be subconsciously ignoring the countless times where we had an injury and felt no pain (or pain not proportional to the extent the injury). We have experienced plenty of bruises and cuts, with little clue on how or when it happened.
Forget the tiny bruises and cuts. It is well known that around 40% of the people admitted to the emergency room with horrific wounds have no pain, and in some, no or low pain even after long delays (1). And mind you, these people are alert, rational and coherent (‘not in shock’ as most people tend to believe). If a crowbar is sticking through your neck or an amputed arm, doesn’t result in pain, why on earth would we think injury is an accurate indicator of pain?
So how could these horrific injuries result in NO pain? As we learned, nociceptors relay danger signals, and it is ultimately up to the brain to produce an output. Most often these horrific injuries happened in a context where survival of the person was at stake, which is a lot more threatening than the injury (ie. focus on the injury or sustain life). And as time goes by and the brain concludes that you are out of danger, it now focusses back on your amputated arm. I cannot work, I cannot lift my kids, I know and have seen amputees struggle, I can see the blood on the bandage: All these beliefs and attitudes and sensory cues are only heightening the fear or threat level of the injury in the brain. And guess what happens now? PAIN.
Now what if your thoughts/attitudes were more positive or less threatening? In 1950 Henry Beecher did a similar study. They wanted to see why soldiers who got injured in war took much less morphine than a civilian or why they had much less pain that expected. The results indicated that it is simply because of “meaning”. For a soldier, despite experiencing a major injury or an amputation, he still survived a war , and could return home and be with his family and friends. The soldiers beliefs and attitude was likely influential over the brains defensiveness, resulting in much less pain than expected (7).
And mind you, these things are happening in a split second and it is outside our conscious control. If you doubt such decisions can be made fast enough, look at the picture below. In fact, both the tables A & B are of the exact same length. Your eyes saw both the tables being the same length, but your brain perceived them being as different lengths in a nano second!
Again, I am writing all this to show that pain is not an accurate indicator of damage and brain constructs pain based on assessing all other inputs. Nociception happens to be just one of those many inputs.
If the brain sends an output of pain, and nociception is just one of the inputs, can we have pain without nociception?
Very good question and the answer is a big yes.
A classic example is phantom limb pain, which has puzzled us for years. In phantom limb pain, forget damage and nociception; people no longer have a body part, yet still feel pain (in their missing body part). Phantom limb pain is a remarkable example of how pain occurs with absence of nociception. We also see plenty of examples around us where people experience pain with no damage or injury.
Now how do researchers study these questions? Here are two popular studies:
- Study 1: The participants in this the study were touched by a cold piece of metal (-20) to evoke a nociceptive response. They were also visually shown one of two colored lights, either red and blue. Before being touched, it was explained that the light was very related to the cold stimulus. Now what did they find? Although the stimulus was identical, 8 out of 10 subjects felt more pain when the red light was shown than blue light. If you think about it, we have learned that red always signals danger. Though there were individual variations, it was very clear that the color of the light changed pain, but not nociception. The nociceptve fibers evoked the same response (as seen by C & A delta fiber activity) under both conditions, but the pain dramatically differed 2 .
- Study 2: Here the subjects placed their head in a sham or fake stimulator and were told a current would run through their head. They were told that the pain will increase as the intensity of the stimulation goes up. As expected, the pain went up as the stimulation went up even though there was no stimulation to begin with. This is another fascinating example of pain without nociception. http://www.ncbi.nlm.nih.gov/pubmed/2038488

As shown above, there are many evolving studies to demonstrate that pain can occur without any damage/nociception/injury.
I don’t care much about the science of acute pain from a cut or a wound. I have chronic low back pain for years due to the 2 herniated discs as shown in my MRI. How does all this brain talk ever change the treatment of chronic pain?
Since now we understood the biology of pain, it is a good time to talk about pain management. As you rightly pointed out, acute pain is pretty straight forward and well understood. As the name implies, it is just acute or short term. We get injured, we ‘may’ feel pain, healing takes over, pain goes away, and we are back to normal (usually 3-6 months). Nobody is really bothered about acute pain, what everyone is worried about is chronic pain.
Chronic pain has always been a mystery to us. Why should this pain last for years and years when injury had enough time to heal? Multiple bullet wounds and major amputations heal within months so why should this tiny injury to your knee or shoulder last for years and years? What do you say?
Or how come there are large numbers of people who have the same dysfunctional tissue but have no pain? We know that around 40% of the population have disc herniations but have no pain whatsoever. And guess what, these people do not end up in pain years later either. This is the exact reason why the American College of Physicians have come forward with clinical guidelines saying ”Clinicians should not routinely obtain imaging or other diagnostic tests in patients with nonspecific low back pain”. We now clearly know that abnormal findings on the x-ray and MRI ( like disc herniations, bulging disk, degenerating joints and so on) are clearly NOT related to the onset, severity, prognosis, or duration of low back pain. If 40% of the general population do have disc hernataions, I do suspect everyone who lifts weights will have one or two disc herniations. 3, 4
Before we understood the role of the brain in pain, we always thought that pain was an accurate indicator of damage and nociception equals pain. So chronic pain always meant that there is an injury yet to be healed. Hence all our treatments were focused on fixing tissue damage and dysfunctions (the biomechanical model). But now we know that in chronic pain, the injury has healed long back and what is maintaining the pain is the sensitive nervous system and the brain. Or in other words, the brain still thinks there is threat and hence still outputs pain.
So yes, all this brain talk has revolutionized the understanding and treatment of pain.
This is interesting, but what the heck do you mean by a sensitized nervous system?
Remember the last time you had a cut or a contusion? Not just the damaged area, but even the surrounding area was very painful even to the slightest of touch (defined as hyperalegisa and alloydynia). What we see here is an increased sensitivity of the nervous system. In other words, both the threshold for activation of the nociceptors is lowered AND the response of the nociceptors is increased. Remember that muscles, joints, skin are just the hardware, the nervous system is the software and where all the action happens.
Now In chronic pain, this nervous system sensitivity is still maintained. The brain believes there is a threat and hence rightly so sends an output of pain. So just flexing your low back with a small weight, which seemed pretty harmless, is now threatening enough to evoke pain.
So the simple goal of any pain treatment is to lower the sensitivity of the nervous system (includes brain).
I see. And how do you lower this sensitivity?
Two ways:
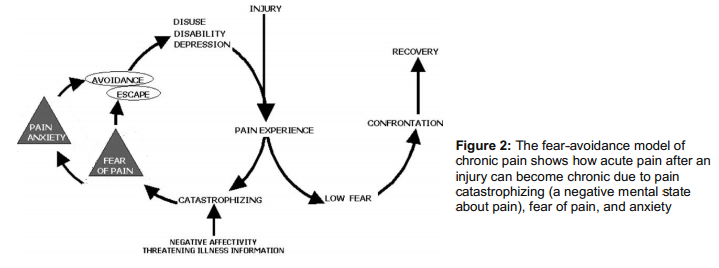
Top Down: Basically, means changing your attitude, beliefs, knowledge (neurophysiology of pain) about your pain and in turn, lowering the threat value of pain. People get hurt, they experience pain, healing follows, and they recover. But in some folks the pain lasts forever. And why is that? According to one of the most well-accepted models - the fear-avoidance belief model - people who have heightened fear of re-injury and pain are good candidates for chronic pain. Lack of knowledge or incorrect knowledge, beliefs ( hurt always means harm, my pain will increase with any activity and so forth), provocative diagnostic language and terminologies used by medical therapists like herniated disc, trigger points, muscle imbalance, and failed treatments can further heighten this fear or threat . So education to lower the threat is THE therapy here. We now have some very good evidence to show that just pain physiology education or the top-down approach is enough to lower pain and improve function 5.
Bottom Up approach: The bottom-up approach is what we see around us: surgery, postural fixing, trigger point, muscle imbalance, movement re-education, manual therapy, acupuncture and the list keeps growing. Almost all treatments out there are trying to lower the nociceptive drive without much consideration to the top-down approach. This is solely because these treatments are based on the outdated model of pain. We now suspect that positive effects of manual therapy may be due to neural mechanisms than the tissue and joint pathology explanations that is often offered. So even the bottom up approach is working via de-sensitizing the nervous system. Although not intended, there are top-down mechanisms clearly at work even in bottom up approaches( like the placebo effect, a credible explanatory model, the belief in the therapist) .
So what we you need is a combined approach that takes into account the “entire individual” and that’s where the biopysycosocial model of pain treatments walks in. The bio psycho addresses the biology (nerves, muscle, joints), psychological ( beliefs, thoughts, fear) and social aspects (work, culture, & knowledge).
So what is wrong with some of the current treatments which are based on the old biomechanical model of pain?
As I wrote, they are just completely based on the bottom-up approach assuming tissue damage and nociception as the sole driver of pain. The is called the ‘find and fix it’ model.
A good question is if it is working, should we worry about all this brain talk?
It is estimated that 1 in 4 people in America are in chronic pain and this was 1 in 7 in the 90’s. So our approach was clearly not working (even if we thought it was). Furthermore, none of our treatments show any specific effects. That means for low back pain: manual therapy, acupuncture, general exercise all seem to elicit similar effects. 6
What is clearly disconcerting is these treatments are given in a context that there is something wrong with the tissues and we need to avoid/prevent /fix it. This structural pathology approach is great to raise the threat level in the brain and in turn maintain or worsen your pain. So even if you get pain relief, you may be nicely setting yourself up for some future pain problems.
Now I am confused. Should I tell people not to use an arched back when they lift because it can raise the threat in the brain? Should I stop foam rolling and other injury prevention methods?
Nope. Just like I wouldn’t advise anyone to cross the street with their eyes closed, I wouldn’t advise anyone to pick a 200 lbs barbell with a rounded back. The age-old simple advice of avoiding extreme loading at the end range of motion still holds good . So proper form is always recommended.
What we don’t want to do is overemphasize or exaggerate our case for injury and pain prevention. For example asking someone to sit with 20% tension in abs, always be upright and never slump, educating disc herniation means the end of the world, knees should never go past toes, spinal rotation is bad and so forth. If you don’t have any clear evidence and you are just speculating, and most are ,it is better to clip that ego and avoid the talk. You can do lot more harm than good.
Should you stop foam rolling and other injury prevention techniques? This is a good question, but a better question to ask is do these really prevent injuries in the first place? Most of the stuff that you often hear are just ‘claims’. If you think those really help, you have sufficient evidence and the client have injury concerns, then go ahead and do it. But what we have to be careful is the language we use to explain these techniques. For example, a better way to present foam rolling is to improve mobility and blood circulation instead of another tool to exorcise out those evil trigger points.
Can we prevent pain?
First, pain is a protective mechanism. If we didn’t have pain, we would be all dead. So pain is normal and necessary. Acute low back pain is as harmless as a common cold and is unavoidable in your life.
Second, what we need to worry about is pain that can become persistent or pain that sustains even after the tissue is healed. And the best way to prevent pain chronicity is to have a better knowledge of pain physiology and how pain is an output of the brain rather than a simple response to injury. It has been shown that people report less pain and less frequently after they receive pain education. Why? Simply because they have lowered the threat level in their brain. Pain education may also serve to lower the pain intensity with acute injuries. So throw away all those unnecessary fears and beliefs about pain and injury.
I am an NASM certified trainer. Our certification emphasizes a lot on postural correction and muscle imbalances. So what about posture?
As I wrote, almost all treatment modalities out there to explain chronic pain is based on the structure-pathology model. We have been studying and researching posture for more than 30 years and we still don’t have any evidence to show posture causes pain. In fact, we have very good evidence to show that posture is not correlated with pain. And If you have been keeping up with me so far, it is not so surprising. Is it?
What we have to understand is pain is just one part of a complex stress response. If you get injured, the body responds by releasing adrenaline, activating large muscle groups to evade threat, deactivating small postural and stabilizing muscles, changing your gait or posture to further avoid injury, slowing digestion, triggering swelling and inflammation and so forth. All makes perfect sense since the body wants to protect and escape from further threat or injury. Once the pain becomes chronic or threat becomes chronic, these complex protective responses are also maintained. You will still maintain those anatalgic or pain evasive postures, your core or postural muscles are still less activated, the over active muscles tend to shorten and become prone to trigger points, swelling and inflammation becomes wide spread and so on. So most of these responses that are often blamed for the cause of our pain are just the consequences of a well-designed, threat response system - posture just happened to be one of them.
I do some postural correction still, but don’t make so many claims as I used to. I just mainly do it for better aesthetics and to improve their function.
What about the strengthening muscles to relieve pain. I thought weak muscles were the problem. I had clients whose low back pain disappeared after doing low back exercises. How come?
Strengthening muscles may or may not have much of an impact on pain. What strengthening is good for is to raise the tissues tolerance, so that you don’t re-injure it. The pain relief people obtain when they do exercises could be very well explained by the non-specific effects of exercise. For example, you have managed to convince and comfort your client that movement is good and not to be feared, especially the body part in question. You also educated them that pain is due to weak or imbalanced muscles and will soon resolve. The improvement in blood flow, performing the actual movement (which was supposedly harmful), the self-belief that he or she will get better all contributes to lowering the threat value in the brain. If you care to notice, these top down and bottom up approaches are common to all movement or exercise based treatments. What is not common is the unique mechanism offered as the rationale for these treatments and their ignorance of the powerful non-specific effects of their treatment.
Once again, although the pain may resolve, we have used an explanatory model that is further instilling the belief that the pain is due to tissue pathology or tissue dysfunction or weakness. And that my friend is not good.
I think that’s all I have. I have omitted a few things, like the pain signature and other pain mechanisms which are a bit more complex. I expect (and hope) this article has raised enough curiosity in you to question some of your own beliefs and understanding about pain and injury.
Anoop.. you have made me really curious. So where can I read more about it?
Thanks!
Great sites to read:
www.somasimple.com (excellent forum)
www.bodyinmind.org
www.forwardthinkingpt.com
www.bboyscience.com
www.saveyourself.ca
www.bettermovement.org
www.thebodymechanic.ca
Great books to read:
Beginner Level
Explain Pain by David Butler & Lorimer Moseley (This is a must read)
Painful Yarns by Lorimer Moseley
Intermediate Level
Pain by Patrick Wall
The Challenge of Pain by Ronald Melzack
Sensitive Nervous System by David Butler
The Back Pain Revolution by Gordon Waddell
Topical Issues in Pain by Louis Gifford
Therapeutic Neuroscience Education: Teaching patents about pain by Adriaan Louw ( a book on how to do the top down approach)
Pain by Lorimer Moseley (DVD)
Acknowledgement:I would like to thank Jason Silvernail DPT, DSc, FAAOMPT and Joseph Brence, PT, DPT, FAAOMPT, COMT, DACc for helping me edit the article. Special thanks to Joe for painstakingly going through the article and making sure everything I wrote is accurate and consistent with the pain science. Please do bookmark his excellent website: www.forwardthinkingPT.com
Please do share this article to everyone you know. It is probably one of the most important articles I ever wrote, and that you will ever read.
Related Articles
Margaretann | Thu January 09, 2014
Well, I know you are partially correct. The pain is in your emotional brain first. If you don’t deal with it it becomes physical ,hence pain. When you come to me ,I unload your hard drive,your brain of the stress at large . The body then allows me to do the osteo mechanics ,I call it that. I then reset tendon ligaments and muscles . No pain. A little psychology , and your back on track. It’s not rocket science ,it’s quantum physics , energy kinesiology, .i get 100percent results every time. No pills, no gimmicks, no doctoring, chiropractors or anyone else just stabbing at air thoughts. I know ,I was hit by 18 thousand pounds and after all the bull rap ,I put myself back together again..like humpy dumpty but better. Doctors said the pain was all in my head. They were partially correct.
Jay-Shian Tan | Thu January 09, 2014
Thanks Anoop!
I’ve been looking for a simple written piece to hand to my patients as I have not had the time to consolidate my thoughts. Your piece is spot on the money, GOOD WORK!
I find the main thing people get wrong is thinking one way to move is the only way to move. Move variably, frequently with acceptable loads in an environment that is comfortable.
-Jay
Enjoyed this. A big part of reducing the threat level is kinesthetic education. I use Hanna Somatic Education with myself and clients, but I’d never considered the impact of the knowledge itself on pain.
Example: tweaked a muscle around my hip whilst squatting on Monday. I’m aware that I can recover through movement and I can set about recovering as soon as I get home. Emotional response to pain is lessened, no undue panic or concern. A big difference in comparison to the novice who tweaks their lower back in training, then jumps straight down the catastrophising route.
Simon MAryanMM, Ph.D. | Thu January 09, 2014
A well researched, thought out and written article. Made for a very interesting read.
Good effort
@Margaretann,
Considering that most highly trained quantuum physicists report signficant levels of uncertainity and a lack of complete understanding, as can be exemplified by an inability to generate a unified theory, what quantuum physics do you think you are using? And how would you propose that said quantuum changes would coincide and relate to known observable changes at the exceedingly more researched and well described biochemical atomic/molecular level and macromolecular (nerve/fMRI)level of science that Anoop’s article is talking about? Also consid ering the ubiquity of quantuumness in the universe how exactly do you consider your self able to harness a particular quality of it and alter it in another structure reliably and consistantly?
Also, considering that it is still unknown how the brain processing level (as described and observed scientifically) and consciousness creation level of experience is related, how do you propose that what is currently considered a distributed level of activity that produces an emergent phenomena can be psycho-located to an ‘emotional’ brain, a structure and process that is neither an anatomically or physiologically accurate description of anything currently known?
In the resetting of tendon/ligament/muscle are you proposing that you use forces to alter connective tissue components, something that requires forces that would result in further lesions, or that somehow using physical level of forces you are able to create a signficant and rapid genetic response with subsequent breakdown and building of connective tissue within a time period that no scientific observation to date has ever witnessed?
When you propose a 100% success rate by what standard do you indicate success?
I am genuinely curious. I am not questioning your faith in your belief, I am questioning your belief’s relationship to signficantly researched and documented science.
Anoop | Fri January 10, 2014
Thanks Mark.
Yep, Margerratann. I am sure you get 100% success.
Thanks Jay! And very good point. When sit for a long time, we get pain, we move and we feel better. We didn’t move to the perfect position. We just simply moved.
Thanks Warren. Good point. You might want to check out Therapeutic Neuroscience Education by Adrian Louw. He does research on the top down approach and how to educate the pain physiology to patients. Moseley has a questionnaire to test people’s knowledge about pain. if I find, I will link it here.
Thank you Simon!
Greg Lehman | Fri January 10, 2014
Hi Anoop,
Super article. Love it.
How do you define disc herniations? Do you mean simple disc protrusions or actual disc extrusions.
Herniations as defined as extrusions are much more rare and I believe (although not sure off hand) may be slightly more relevant to the pain experience than simple protrusions.
Quick reference here by Stadnik
Greg Lehman | Fri January 10, 2014
As a follow up, I remember a similar study suggesting that disc extrusions may be more prevalent in those with pain than in asymptomatics.
The study below is not the one I recall but it is similar. In summary, while simple protrusions arent related to pain a greater degree of mechanical disruption of connective tissue (an extrusion) may be better related to pain.
http://www.ncbi.nlm.nih.gov/pubmed/8747239
None of this takes away from your message but there often seems to be some threshold (modifiable as it is with other factors in the Neuromatrix) where the extent of tissue disruption is related to nociception and subsequently pain.
Anoop | Fri January 10, 2014
Thanks Greg for the comment.
I haven’t done that much research to speak in-depth about it. I just hope this article to be a good introduction to pain science and help trigger some curiosity. And I don’t think it will change much of the main message of the article as you wrote.
And not sure how I forgot your site. So added it!
Stefanie Foster, PT, FAAOMPT | Fri January 10, 2014
I like the way you’ve written this. This is a very important topic, but too often, I see professionals trying to take sides as if you have to be all top-down or all bottom-up. Even doing your due diligence to educate and go top down, certain people may dismiss it at first, but you’ve planted a seed that may later grow to bear fruit! I think somatic psychologists (such as Peter Levine’s Somatic Experiencing) are very well suited to help people through escaping the fear-avoidance loop and I often recommend that for my patients.
John Feil PT, DPT, OCS | Sat January 11, 2014
Excellent article. I just gave a lecture about pain to seniors yesterday and alot of what you talked about in the article is what I presented.
Keep up the good work.
Anoop | Sat January 11, 2014
Thank you Stefanie!
I completely agree. And you took the exact words out of my mouth; all I am hoping is to plant a seed in their minds. I think this a really important topic for fitness professionals. Even if we don’t help, we shouldn’t make the problem worse!
Thanks John. I appreciate you taking the time to comment. I remember reading that thread in somasimple. Next time, you should give them the pain questionnaire before and after and see how much they improve. That would be perfect.
Great article. Thanks.
There is one change you may want to make. Although bodyinmind.com may be a great site to read, I don’t think it is applicable to your article. I think you meant bodyinmind.org
Anoop | Sun January 12, 2014
Thanks Chris for the comment.
haha. Thanks for the catch. I remember in one of the presentations Moseley talking about someone accidentally showing the .com website in front of a big crowd.
Anoop | Mon January 13, 2014
Thanks Anatoly! I agree a bit long, but wanted to give the full scoop.
Kyle Norman | Fri January 24, 2014
Anoop,
Thanks a lot for writing this. I just found your site via Soma Simple and I’m very eager to read through it. I’m a personal trainer/strength coach who recognizes this biopsychosocial model for pain. Sometimes I struggle to explain this to people and you’ve done the job for me.
I started out with the pure biomechanical model for pain, was introduced to the current neuromatrix/neuroplasticity/threat modulation ideas through Z-Health (I know Z-Health has been ripped apart on Soma Simple, still that’s where I first was exposed to modern pain theories) then I returned back to the biomechanical stuff—and now I’m back to the updated pain model(s). Anyway, I’m trying 1) do the best I can for my clients and 2) learn. This article has been a very good 2nd helping of some of the things I learned a few years ago. Thanks again for all this good info.
Anoop | Sat January 25, 2014
Thanks Rbob!
Thanks Kyle!Everyone, including me, started out with the pure biomechanical model.So I do understand where you are coming from. It is for people like you I wrote this one so thanks for sharing your thoughts.
prohormones | Fri January 31, 2014
Impressive weblog Anoop. I am going to give a presentation on bodybuilding and fitness. Reading your article is very helpful to me. Thanks a lot!
Fascinating - because I lived this.
I was healthy, energetic, vibrant, and pain-free 15 years ago. I started going downhill, and within a matter of weeks had body-wide pain, extreme fatigue, blurred vision, tinnitus - too many symptoms to list them all. I was dx with fibromyalgia and was pretty miserable for 10 years, until I was tested for celiac disease. After removing gluten from my diet, I felt worlds better, but the body-wide aching remained. Then I read a book - The Great Pain Deception - recommended by a friend. Today I am pain free and healthy. If I could only convince my brain that I don’t have celiac disease and could eat a normal diet - that would be perfection!
Anoop | Fri September 05, 2014
Thank you Sue for the comment.
ken hoffer | Fri September 05, 2014
I think that you are seeing a bit of what chiropactors experience. For almost 100 years we have had interest in the pain field but the public and health professions do not wish to listen and learn. I’m fairly sure that we offer some competition in the field but we are always denigrated for our work. School is 4 years of intense basic sciences plus all health related subjects. Needless to say’ one must learn something in that span of time. The schools say we are doctors, and the states and federal boards agree. Just take a look at the state board examinations we have to be licensed and you will get an idea of our education. It goes without saying that the nervous system is supreme in controlling much of the bodies functions and chiros work intimately with that system. Its past time for recognition and approval from other professions. I had hoped to see it in my lifetime but it is coming slowly.
Thank you
Steve Feinberg | Wed March 02, 2016
I really enjoyed this read, Anoop, and much of the follow up commentary in this discussion thread. Question: is the same thought process (top down) being studied to this extent as well in order to facilitate healing from illness and internal inflammation rather than blanketing with medication? I’m wondering if proof is rendered that this model applies. Can we become less sick the same way we can become less hurt? I have always believed in the power of the mind, and it has shown plenty of correlation to healing in studies over time, but having a model like the one you’ve shown above that would connect the scientific process of perception and elimination of some sickness. I would suppose the ones that would be first on the list (conditions, some referred to as diseases) would include fibromyalgia, mono, walking pneumonia, things that deal with immunity/fatigue/inflammation as well as bacteria/virus/irregular or atypical tissue activity? I’m open to all educated comments and opinions here, thirsty for knowledge, please excuse any of my ignorance in advance:-).
Anoop | Fri March 18, 2016
Hi Steve,
Thank you so much and sorry for the late reply.
That is a good question. And I think there is some proof when it comes to stress and inflammation. I think a lot of the problems in our understanding comes from our habit of breaking whole into parts and studying them as separate/isolated parts. For example, now its very clear in pain that your brain affects your PNS and PNS affects your brain. It is one system .We just happen to divide it so WE can understand it better.
Thank you
Anoop
Aaron Allen | Thu October 19, 2017
Mostly a great article. Many strawman arguments about what manual therapists supposedly believe/are mis-explaining to clients. I was taught the same scientific evidence expressed here by the author during my massage therapy education a decade ago. Author seems to grab onto some people’s historical mis-understandings of posture, mechanics and pain, and paints entire professions as unable to integrate the newer science, even as his own field has been forced to do the same.
Aaron Allen | Thu October 19, 2017
I may have posted my comment to the wrong article. I was attempting to answer an article by this same author which appears to be a variation on this theme.
Brian Reddy | Wed April 25, 2018
Hey Anoop,
“So education to lower the threat is THE therapy here. We now have some very good evidence to show that just pain physiology education or the top-down approach is enough to lower pain and improve function 5.”
This study you cite (5) was a research review on pain education.
It was done by an author who sells a book on pain science education.
Five out of the eight studies reviewed were done by this author’s coauthor of that very pain science education book. Five out of the seven RCTs -the studies we put the most faith in- were done by this coauthor.
These two authors also run an entire business -books, courses, speeches- around pain science education.
Hey, I think Moseley and Butler have great information. I’m a happy customer of multiple products, and I give some pain science education to every new client, but nobody is immune to conflicts of interest. Worse, this conflict should have been disclosed in the paper. (Whenever a conflict isn’t mentioned, the suspicion radar beeps louder.)
For the other three non-Moseley studies:
-one found the effect of pain education leveled off at three months
-one looked at whether a 30 minute intervention improved immediate understanding of pain science i.e. it asked some questions after the 30 minute session. It had no other follow up. They list this as a major limitation: “This is in fact the most important limitation of the present study: the lack of a follow-up period in which both information retention and changes in cognitions or behavior could be evaluated.”
Plus, it was done in chronic fatigue syndrome patients. Not really applicable to the fitness practitioner’s clientele of a localized painful knee.
-The last study had a sample size of 6. I mean, the other two above had sample sizes of 38 and 46. Not exactly great. But 6?!
-All three studies used Butler and Moseley’s “Explain Book” as the pain science education. In other words, Butler did a review on eight studies assessing whether his own book / business works.
Back to the overall review- it states in the studies it reviewed, pain education was done in conjunction with other treatments. Thus,
“Based on the lack of consistent control groups in the articles reviewed, it is not possible to draw strong conclusions about the influence of the NE content versus individual attention and the acknowledgment that perceived pain may be real.”
Even with all the conflict of interest, your takeaway is stronger than Butler’s!
More succinctly: recent research, from this month, from pain scientists, state, “studies evaluating pain neuroscience education alone report small effect sizes. (28)” That (28) referenced is actually the same Butler review.
That study: Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor Control Training on Chronic Spinal Pain A Randomized Clinical Trial
They found used in conjunction with exercise (they actually used quite a bit of Sahrmann techniques), results are much better.
I don’t mean to sound combative, but this is a consistent issue in the pain science world. The concomitant followers over embellishing, often much more than even the people who’ve come up with the techniques.
Anoop | Thu April 26, 2018
Hi Brian,
Thank you for the comment.
1.Butler is the 3rd author and probably contributed the least based on the author sequence. It is Adrian’s paper. First author contributes most of the work and does most of the writing. So just don’t call it Butler’s paper again and again.
2. Moseley is not a NOI instructor or involved in NOI group. Writing a book or giving speeches in your field or area of interests is pretty common for most researchers/faculty these days. What else are they goona speak/write about? And the royalties/honorarium they get is peanuts. Your argument that Moseley’s articles cannot be counted don’t have much merit. Butler is the director of NOI group and should have included in the COI that he seems to have done in other articles.
3. The sample size with 6 subjects is a pilot study as written in the title of the article. And a good systematic reviews should all includes all articles irrespective of their sample size/quality
3. The conclusion of the article states” For chronic MSK pain disorders, there is compelling evidence that an educational strategy addressing neurophysiology and neurobiology of pain …. ” My conclusion is very much consistent that article conclusion. And this is a blog post for lay people in layman’s language and a gentle introduction to the pain science. It is not a in-depth review of the literature on pain education.
4. “They found used in conjunction with exercise (they actually used quite a bit of Sahrmann techniques), results are much better.”
And if you read my article, that’s pretty much I talked about in my article. Using BOTH top down and bottom up approach: From the article” So what we you need is a combined approach that takes into account the “entire individual” and that’s where the biopysycosocial model of pain treatments walks in. The bio psycho addresses the biology (nerves, muscle, joints), psychological ( beliefs, thoughts, fear) and social aspects (work, culture, & knowledge)”
And here is the conclusion of the recent JAMA article you posted” This finding emphasizes the need for a shift toward a biopsychosocial focus (ie, cognition and perceptions underlying the pain problem), rather than maintaining a focus toward a purely biomedical origin when treating these patients in clinical practice.” Happy to say this is exactly what the theme of my article is.
“I don’t mean to sound combative”
You are not combative. You are just little frustrated as is expected from someone who is attached (emotionally and financially) to the biomechanical model of pain. I can’t help notice that you sell almost half a dozen books based on posture and dysfunctions. So I understand.
Anyway, thank you for the JAMa article
Brian Reddy | Wed May 02, 2018
1) Of all the responses to my comment, I thought debating whether there was a conflict of interest was pretty far down on the list.
While I didn’t say it was solely Butler’s paper, after all, few research articles are written by one person these days, so I thought that’d be implied, especially considering how many with PhDs are here, but I could see how it seemed I suggested Butler was the only author. Fair enough.
Beyond that, on the COI point, like you trying to guess how much influence Butler had, we’ll have to agree to disagree.
2) I never said Moseley’s articles don’t count. Nor did I say a conflict of interest automatically disqualifies a study’s validity. It’s why I made a point of saying I’m a happy customer of theirs. But you saying there is “very good evidence” was not backed up with such.
3) Lol, oh geez, I had a feeling you’d go ad hominem here. Also, I appreciate the irony in you saying I have a conflict of interest. I promise you I made less money from this blog comment than Butler makes on royalties!
Hey, if you want to come at me personally, that’s fine. I’m quite comfortable in the results I’ve had, with a pretty big page of testimonials to back it up. Plus, if you read around the site more, you’ll find your points are misguided. Butler and Moseley are on my recommended personal training reading list, I cite tons of Moseley studies, I reference how much emotions can play a role in recovering from surgery, literally every program I give to people incorporates weekly graded motor imagery, yada yada. You can come at me saying I don’t apply pain science in the exact manner you wish, but you can’t come at me acting like I’m unaware of the topic.
And you specifically asked I come read this page! It’s not like I walked in here randomly with an axe to grind.
If I have any frustration, it’s whenever I read the research pain science blogs cite, they’re pretty far off from what the actual research says, or how the real world operates.
As another quick point: many in this community act like orthopedists have no concept of the lack of relationship between structure and pain. I’ve had orthopedists as clients. They’re well aware. I’ve gone into operating rooms with them and seen them specifically leave bone spurs alone because “that’s not giving them any issues.” We have research at least as old as 1994 illustrating this awareness: https://www.nejm.org/doi/pdf/10.1056/NEJM199407143310201 .
(I also happily acknowledge there are some who obsess over structure too much.)
We can let others make up their own mind for whether a misinterpretation in research happened here, but I wanted to point out a different opinion. Thanks for letting me voice it. I think the thesis and main takeaway of your post, and many pain science blogs, is solid. But the initial premise -everybody is ignorant of this topic except a few in the know- and other details are often flawed or lacking.
This is evidenced by the fact the pain science community has had an awfully hard time communicating this topic well. (I know I was very confused myself until I started reading all the papers.) Again, ironic considering communication is a major tenet of the practice.
This is a point you make in your introduction. If you simply said “Different people experience pain differently, we need to account for this when people are in pain,” which I’m not sure anybody has a problem with, and, while not revolutionary, you’d get a lot more head nods.
Be Serious | Sun November 04, 2018
“But now we know that in chronic pain, the injury has healed long back and what is maintaining the pain is the sensitive nervous system and the brain. Or in other words, the brain still thinks there is threat and hence still outputs pain.”
How does this theory of chronic pain relate to the pain of chronic migraine? What is the “threat?” And what was the “injury” that “healed long back?”
Oh wait. It’s not a theory. It’s what “we know.”






